A stress fracture is a small crack in a bone. Stress fractures often develop from overuse, such as from high-impact sports like distance running or basketball. Most stress fractures occur in the weight-bearing bones of the foot and lower leg. Studies show that athletes participating in tennis, track and field, gymnastics, dance, and basketball are at high risk for stress fractures. In all of these sports, the repeated stress of the foot striking the ground can cause problems. Rest is the key element to recovery from a stress fracture.
Description
A stress fracture is an overuse injury. When muscles are overtired, they are no longer able to lessen the shock of repeated impacts. When this happens, the muscles transfer the stress to the bones. This can create small cracks or fractures.
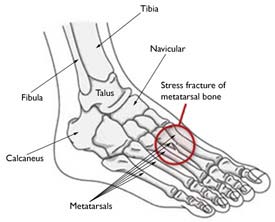
The most common sites of stress fractures are the second and third metatarsals of the foot. Stress fractures are also common in the heel (calcaneus), the outer bone of the lower leg (fibula), and the navicular, a bone on the top of the midfoot.
The most common sites for stress fractures in the foot are the metatarsal bones.
Cause
Stress fractures usually occur when you increase your high-impact activity by:
- Frequency (how often you exercise)
- Duration (how long you exercise)
- Intensity (your level of exertion)
People who do not exercise can also have stress fractures. If osteoporosis or other disease has weakened bones, normal daily activities may result in a stress fracture. This is called bone insufficiency. It is one of many factors that can increase your risk for stress fracture.
Conditioning
Doing too much too soon is a common cause of stress fractures. For example, runners who are confined indoors for the winter may want to pick up where they left off at the end of the previous season. Instead of starting slowly, they try to match their previous mileage. Because of the lower level of conditioning, muscles become fatigued faster. The result could be a stress fracture in the foot or ankle.
Those who are new to exercise and try to do too much too soon are also at risk.
Equipment and Environment
Improper sports equipment, such as shoes that are too worn or stiff, can contribute to stress fractures.
A change of surface, such as going from a grass tennis court to one of clay, or a change from an indoor to an outdoor running track, can also increase the risk.
Technique
Errors in training or technique are another cause of stress fractures. Anything that alters the mechanics of how the foot absorbs impact when it strikes the ground may increase your risk for a stress fracture. For example, a blister, bunion, or tendonitis can affect how you put your weight on your foot, and may require a bony area to handle more load than usual.
Bone Insufficiency
Insufficiency stress fractures result when the bone itself is weak. Conditions like osteoporosis reduce bone strength and density. This increases the risk of fracture.
Anyone with a medical problem or taking medication that decreases bone density is susceptible to stress fractures.
Female athletes who experience irregular or absent menstrual periods may also have decreased bone density. Studies show that female athletes are more prone to stress fractures than their male counterparts are. Many doctors attribute this to “female athletic triad.” This three-sided condition includes eating disorders, irregular menstrual cycle, and osteoporosis. As a woman’s bone mass decreases, her chances for getting a stress fracture increase.
Symptoms
- Pain that develops gradually, increases with weight-bearing activity, and diminishes with rest • Pain that becomes more severe and occurs during normal, daily activities
- Swelling on the top of the foot or the outside of the ankle
- Tenderness to touch at the site of the fracture
- Possible bruising
Doctor Examination
Medical History and Physical Examination
During the first visit, your doctor will ask you about your work, your activities, and any medications you take. It is important that your doctor understands what your risk factors for stress fractures are.
After discussing your symptoms and medical history, your doctor will examine your foot and ankle.
Imaging Tests
Imaging tests may help your doctor confirm your diagnosis.
Stress fractures are difficult to see on X-rays until they have actually started to heal. Your doctor may recommend a bone scan or a magnetic resonance imaging (MRI) scan, which are more sensitive than an X-ray and can detect stress fractures early.
Treatment
First Aid
If you suspect a stress fracture in your foot or ankle, stop the activity and rest. Ignoring the pain can have serious consequences. The bone may break completely.
Apply an ice pack and elevate your foot above the level of your heart. Nonsteroidal anti-inflammatory medicines like ibuprofen or naproxen may help relieve pain and swelling, but may inhibit bone healing. Try not to put weight on your foot until after you see a doctor.
Nonsurgical Treatment
Treatment will vary depending on the location of your stress fracture and its severity.
The goal of any treatment is to help you return to all the activities you enjoy. Following your doctor’s treatment plan will restore your abilities faster, and help you prevent further problems in the future.
Rest. Take a break from the activity that caused the stress fracture. It typically takes 6 to 8 weeks for a stress fracture to heal. During that time, switch to aerobic activities that place less stress on your foot and leg. Swimming and cycling are good alternative activities. Remember, however, that you should not do any physical activity on the involved foot or ankle until you consult a doctor. Protective footwear. To reduce stress on your foot and leg, your doctor may recommend wearing protective footwear. This may be a stiff-soled shoe, a wooden-soled sandal, or a removable short-leg fracture brace shoe.
Casts. Stress fractures in the fifth metatarsal bone (on the outer side of the foot) or in the navicular or talus bones take longer to heal. Your doctor may apply a cast to your foot to keep your bones in a fixed position and to remove the stress on your involved leg. Casts are a type of external fixation. To keep weight off your foot and leg, your doctor may recommend that you use crutches until the bone heals.
Surgical Treatment
Some stress fractures require surgery to heal properly. In most cases, this involves supporting the bones by inserting a type of fastener. This is called internal fixation. Pins, screws, and/or plates are most often used to hold the small bones of the foot and ankle together during the healing process.
Recovery
Once your stress fracture has healed and you are pain-free, your doctor will allow a gradual return to activity.
Slow pace. During the early phase of rehabilitation, your doctor may recommend to alternate days of activity with days of rest. You should slowly increase the frequency, duration, and intensity of your exercise. If the activity that caused the stress fracture is resumed too quickly, larger, harder-to-heal stress fractures can develop. Reinjury could lead to chronic problems, and the stress fracture might never heal properly.
Cross-training. Varying the types of aerobic exercise you do may help you avoid repeated stress on your foot and ankle.
Prevention
These guidelines can help you prevent stress fractures.
- Maintain a healthful diet. Eat calcium and vitamin D-rich foods to help build bone strength.
- Use proper sports equipment. Don’t wear old or worn running shoes.
- Alternate your activities. For example, you can alternate jogging with swimming or cycling.
- Start any new sports activity slowly. Gradually increase time, speed, and distance; a 10% increase per week is fine.
- Strength training can help prevent early muscle fatigue and prevent the loss of bone density that comes with aging.
- If pain or swelling returns, stop the activity. Rest for a few days. If pain continues, see your doctor.
Codeveloped with the American Orthopaedic Foot and Ankle Society
Co-developed with the American Orthopaedic Society for Sports Medicine
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS “Find an Orthopaedist” program on this website.
program on this website.