Why are steroid injections used in the upper extremity?
Steroid injections are commonly used to treat a variety of inflammatory conditions the upper extremity. Examples of these include trigger fingers (stenosing tenosynovitis), De Quervain’s tendonitis, carpal tunnel syndrome, arthritis, tennis epicondylitis), and rotator cuff tendonitis (see Figure 1).
What is in a steroid injection?
Steroid injections typically contain a mixture of a synthetic cortisone and a local such as lidocaine or bupivacaine. Cortisone is a steroid normally produc adrenal gland and is a powerful anti-inflammatory. There are several availabl preparations such as triamcinolone, betamethasone, and dexamethasone are also commonly referred to by their trade names. They all have similar m although they vary in strength and duration of action (short versus long-acting) preparation has been found to be superior to others so the choice of medic up to the individual provider. These anti-inflammatory steroids are distinctly dif the anabolic steroids that have been abused by some athletes for body-bu performance enhancement. The local anesthetic dissolves the steroid and an the area of the injection, diminishing discomfort during the procedure.
How does it work?
Steroid injections work by decreasing inflammation. Once the inflammation the associated pain usually improves as well.
How is the procedure performed?
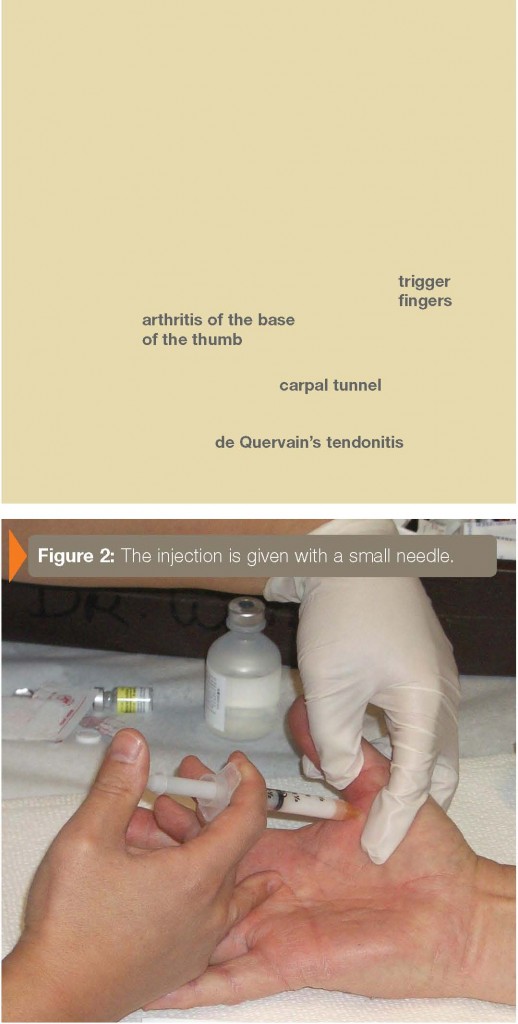
The area to be injected is first cleansed with an antiseptic such as an iodine pr alcohol, or other skin disinfectant. The injection is then given with a small needle Figure 2). Typically, only a small amount of steroid and local anesthetic is Afterwards, the area is covered with gauze or an adhesive bandage.
When does it take effect and how long does it last?
The injection should take effect within a few days and the benefits can last weeks. The exact timing, however, varies from patient to patient. For some conditions, one injection can be sufficient to completely get rid of the inflammation and for more severe cases, several injections may be required. Most patients respond to injections although a small subset may not experience any relief of symptoms.
How many injections can one get?
There is no set rule as to how many injections a person can get. Many providers three injections as a rule of thumb although, in some cases, more frequent may be helpful. Your response to the first injection is very important in determining whether to proceed with re-injection: If the first injection doesn’t work or quickly it may not be worthwhile repeating. Many providers limit the number of because repeated cortisone may cause damage to tendons and/or cartilage.
What are common side effects?
The most common side effect is known as a cortisone flare. This is thought to happen when the steroid crystallizes after being injected. In patients who experience a flare, a brief episode of pain lasting one or two days follows the injection. This pain can be worse than the initial discomfort for which the injection was given. Cortisone flares resolve spontaneously over a few days and can be treated with ice and immobilization.
Another common side effect, especially in patients with darker skin, involves skin discoloration at the injection site. The skin becomes locally lighter in color and sometimes thinner. Although this can improve, the whitening of the skin can sometimes be permanent.
One of the more serious complications from steroid injections is an infection, especially if the injection was given into a joint. Fortunately infections are rare and can usually be prevented by carefully cleaning the skin before performing the injection. Very rarely, some patients may experience allergic reactions to the steroid or local anesthetic in the injection.
Concerns in diabetic patients
Patients with diabetes will often notice a transient increase in their blood glucose in the days following a steroid injection.
When should you call your health care provider?
If you have received a steroid injection and the area is bright red, warm to the touch, or your temperature is greater than 101° orally, you should call your provider to check for an infection.
American Society for Surgery of the Hand • www.handcare.org